Can an ileostomy cause iron deficiency?
When you’ve had ostomy surgery, it’s normal to worry about becoming deficient in vital nutrients that your body needs. In this case, I am going to talk you through my experience with iron-deficiency anaemia after ileostomy surgery. I’ll talk you through the signs, symptoms and the treatment I have received, all based on my experience and my own understanding.
What is iron-deficiency anaemia?
Iron deficiency anaemia is a common type of anaemia. With this type of anaemia, the blood doesn’t have enough healthy red blood cells. Red blood cells are the cells which carry oxygen round our body. Without enough iron, the body can’t produce enough haemoglobin. Haemoglobin is the substance that enables the blood cells to carry oxygen.
Why can having your large intestine out cause iron-deficiency anaemia?
In my experience and learning only, some parts of having an ileostomy and Crohn’s disease can be:
- Not getting enough iron in your diet due to limiting certain foods with an ileostomy such as red meat and green, leafy vegetables. This depends on what you can eat with an ileostomy as everyone is different.
- Having to alter your diet due to Crohn’s disease can also impact whether you get enough iron in your diet.
- Having an ileostomy and/or Crohn’s can also reduce the ability of your small intestine being able to digest iron back into your bloodstream, especially if you are in a flare-up or have had some of your small intestine out. If you are in a flare-up, blood loss can also contribute to this.


- Iron-deficiency anaemia can also be a common side effect of having inflammatory bowel disease, in general.
It is stated (here) that iron-deficiency anaemia “is a common problem, with just under half of people (42%) with Crohn’s developing anaemia within a year of their diagnosis.”
What are the signs and symptoms of iron-deficiency anaemia?
Symptoms can include:
- Tiredness and lack of energy
- Shortness of breath
- Noticeable heartbeats (heart palpitations)
- Pale skin
Less common symptoms can include, but aren’t limited to:
- Headaches
- Food tasting strange
- Feeling itchy
- A sore tongue
- Hair loss – typically noticing more falling out when brushing or washing it
- Finding it hard to swallow (dysphagia)
- Painful open ulcers at the corners of your mouth/lips
- Restless legs
How do doctors diagnose iron-deficiency anaemia?
Diagnosing iron-deficiency anaemia is thankfully quite straightforward with a simple blood test. Your doctor will normally ask for a full blood count (FBC) to be analysed which will check if the number of red blood cells in your blood is normal. Preparation for this test is non-existent and the test will also check for other types of anaemia. Iron deficiency anaemia is one of the most common forms of anaemia but there are also other types such as vitamin B12.
What treatment is there for iron-deficiency anaemia?
- It is important that the underlying cause is looked into, i.e. to determine where blood loss is in the body, and this should be treated wherever possible
- I experience heavy periods and take tranexamic acid tablets when on my period to increase blood clotting. This slows the bleeding down and I’ve found it also helps with my pain as a result of this.
- Iron tablets and liquid. These can cause side effects, i.e. tummy ache, constipation or diarrhoea, black poo, feeling sick and heartburn. I take liquid iron with my ileostomy as I find my digestive system can tolerate this better, although it can make my ileostomy output runnier and more frequent.
On iron treatment, blood tests are then usually repeated every 3 months (for example) to check the iron levels in your blood.
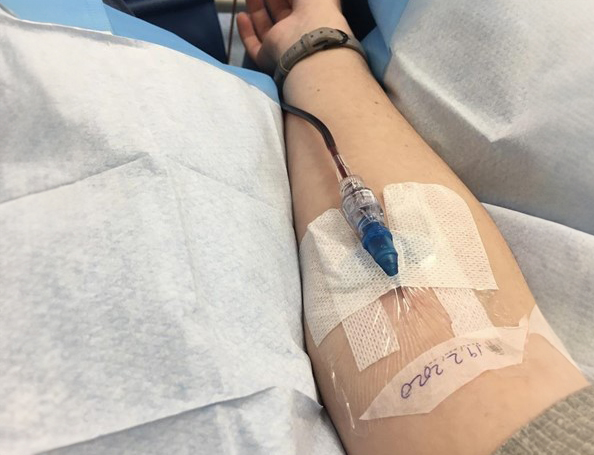
Iron infusions: Sometimes, where your iron stores (base levels of iron) are too low or you can’t tolerate other iron treatment, iron infusions may be given in hospital as a day patient. Usually, these can be done relatively quickly. The last one I had was in 2020.
Things you may be able to do yourself for iron-deficiency anaemia
Always speak to a doctor before trying to treat iron deficiency anaemia yourself. In general, the following things may help:
- Everyone is different – approach with caution with an ileostomy and be aware of signs of an obstruction and/or unwanted side effects if you are going to try and treat this with diet.
- Keep a food diary. This way, if you encounter a problem, you are more likely to track the cause.
- Iron-rich foods include: dark green vegetables, i.e. kale, cereals and bread with extra iron in their ingredients (fortified), meat, dried fruit such as raisins and apricots, pulses (beans, peas and lentils) – again, a lot of these can cause problems for those with an ileostomy, small amounts. Try one new food at a time and chew, chew, chew! Trying one new food at a time helps you to isolate the cause of any issues that should arise.
- You may be recommended to drink less tea and coffee. You may also be advised to eat less dairy and milk and foods with high levels of phytic acid, i.e. wholegrain cereals which can stop your body being as efficient at absorbing iron.
- Smoothies may be a good way to get iron-rich fruit and vegetables into your diet in a more digestible format. Note that these may also speed your ileostomy output up, as well as make it thinner.
If you have any symptoms of iron-deficiency anaemia and/or are concerned, always speak to a doctor. Everyone has different experiences with having bowel disease and/or an ostomy, so it is important to remember this. Thankfully, iron-deficiency anaemia does have solutions for most people. If you have any symptoms of iron-deficiency anaemia and/or are concerned, always speak to a doctor. Everyone has different experiences with having bowel disease and/or an ostomy, so it is important to remember this. Thankfully, iron-deficiency anaemia does have solutions for most people.
Thank you for reading!